Ingvild Bjellmo Johnsen, Medical Advisor on the ERS congress
The European Respiratory Society’s international congress opened on Saturday, Sept 9 in Milan, which is home turf for the family-owned company Chiesi. This year’s congress theme is Pollution, climate change and sustainable developments – which undoubtedly is strongly linked to our outlook on lung health for generations to come.
Chiesi’s Nordic medical team has been in Milan to collect all the gold nuggets from the extensive program and are excited to share our congress highlights with you! We hope that this reading will bring you inspiration and food for thoughts.
Ciao!
Warm greetings from the Nordic Medical Team
Update from the International Respiratory Coalition
Wednesday morning, a much-changed Milan and ERS appeared: the temperature had dropped, there was light rain, the city smelled of flowers and green grass, and a scarcity of people in the huge conference convention. All the voices, faces, queues and noise of the hard-working ventilation – soon just a memory.
COVID-19 – a fading memory?
The International Respiratory Coalition (IRC) presented its work, and we were reminded that the world suffered from the COVID-19 pandemic just two years ago, but even that memory seems to be fading. The political area lost the knowledge of the pandemia, says Tobias Welte, Hannover, Germany. The next pandemic will, no doubt, come at some point in time, and we must not miss the chance to be better prepared. The IRC was initiated to develop ways to tackle hazards for health care in the respiratory field.
While during the COVID-19 pandemic an increased life expectancy in people living with chronic respi- ratory conditions was observed1, re-prioritisation of health care resources also reduced the chances of survival in case of hospital admissions2. Hospital mortality of an acute COPD exacerbation, Welte reminds the audience, is 5%, while 30% of persons experiencing an acute exacerbation of their COPD will be re-admitted to hospital. This comprises huge consequences for people and healthcare. Moreover, during the pandemic, more people died due to de-prioritised or delayed care of conditions like lung cancer, cardiovascular diseases or other comorbidities3. Exacerbation rates in COPD became higher than before4.
COPD: cheaper to stick to guidelines
Marc Miravitlles, Spain, showed numbers on the financial impact of low adherence to treatment guidelines in COPD5,6, underlining the societal costs related to exacerbations. One COPD exacerbation has been shown to be a prognosticator for the next exacerbation7. Susceptibility to exacerbations in defined groups of persons and prognostics risk factors are known, thus, Dr. Miravitlles concludes: “We know whom we shall concentrate our efforts on in the first place”.
Wildfires, a burning health topic
More threats to global lung health: Christine Jenkins, Sydney, Australia, shows scientific evidence of the devastating impacts of wildfires on health: wildfire smoke is recognised for its toxicity, partly caused by the immense amount of respirable particulate matter. The frequency of wildfires increases after periods of dryness, and as we remember from pictures in the newspapers during summer 2023, wildfires are not limited to Australia or America, but occur in Europe. This gives rise to short and long-term consequences for lung health8:
Again, persons living with respiratory conditions are extra vulnerable in such environments, as shown by the increased need for oral corticosteroids9. Wildfires release greenhouse gases also contributes to global warming.
So, what can be done NOW to be better prepared for the future?
HEPA filters: For the threats caused by wildfires, use of HEPA filters as well as recommendations for vulnerable groups (children, pregnant women, elderly, and persons living with asthma and/or COPD) to wear face masks and assure valid rescue medication at home were discussed during the presentation.
Vaccinate: The importance of preventive vaccinations cannot be overemphasised, as it has been shown to both reduce morbidity and mortality10. Furthermore, there is still a need to improve diagnosis of COPD, primarily using spirometry, and with this, to identify persons with increased health risks.
Communicate: In the capacity as representative of GAAPP, an international coalition of 108 patient advocacy groups, Tonya Winders, Hendersonville, USA, emphasised the patient ́s perspective:
we were presented with a clear communication on what matters for patients with respiratory conditions.
We need to look at the person, not just the patient or the diseased organ, says Winders.
Moreover, mortality, morbidity, knowledge of risk factors, and communication matters to patients. She expands the point of the importance of communication and demands information in native languages, taking cultural adaptations into account, and the use of lay language. “Talk as if you were addressing a ten-year old.” As parts of the world are challenged in literacy, reliable digital health information is important, eg. collaborations with YouTube Health or the use of chatbots to manage chronic disease.
What can YOU yourself do?
Educate yourself: More suggested actions can be found in the paper “Climate change and respiratory disease: clinical guidance for healthcare” (see recommended reading).
Organize. If existing channels/organizations can be used to create more impact, use your voice. The IRC is welcoming actions to prepare healthcare for future challenges, but the IRC does not (yet) have national committees in the Nordic region. However, the IRC offers help and support to form one. Go to https://international-respiratory-coalition.org and find the “Join us” form.
Recommended reading:
IRC manifesto:
https://international-respiratory-coalition.org/ wp-content/uploads/2023/06/IRC-Manifesto-Final.pdf
Andersen ZJ, Vicedo-Cabrera AM, Hoffmann B, Melén E. Climate change and respiratory disease: clinical guidance for healthcare professionals. Breathe (Sheff). 2023 Jun;19(2):220222. doi: 10.1183/20734735.0222-2022. Epub 2023 Jul 11. PMID: 37492343; PMCID: PMC10365076.

Barbara Fuchs,
Medical Manager, Chiesi Nordic
References
- Alqahtani JS, Oyelade T, Aldhahir AM, Mendes RG, Alghamdi SM, Miravitlles M, Mandal S, Hurst JR. Reduction in hospitalised COPD exacerbations during COVID-19:A systematic review and meta-analysis. PLoS One. 2021 Aug 3;16(8):e0255659. doi: 10.1371/journal.pone.0255659. PMID: 34343205; PMCID: PMC8330941.
- Gallo E, Prosepe I, Lorenzoni G, Acar AŞ, Lanera C, Berchialla P, Azzolina D, Gregori D. Excess of all-cause mortality is only partially explained by COVID-19 in Veneto (Italy) during spring outbreak. BMC Public Health. 2021 Apr 26;21(1):797. doi: 10.1186/s12889-021-10832-7. PMID: 33902527; PMCID: PMC8072094.
- Magnani C, Azzolina D, Gallo E, Ferrante D, Gregori D. How Large Was the Mortality Increase Directly and Indirectly Caused by the COVID-19 Epidemic? An Analysis on All-Causes Mortality Data in Italy. Int J Environ Res Public Health. 2020 May 15;17(10):3452. doi: 10.3390/ijer- ph17103452. PMID: 32429172; PMCID: PMC7277828.
- Liao KM, Chen YJ, Shen CW, Ou SK, Chen CY. The Influence of Influenza Virus Infections in Patients with Chronic Obstructive Pulmonary Disease. Int J Chron Obstruct Pulmon Dis. 2022 Sep 14;17:2253-2261. doi: 10.2147/COPD. S378034. PMID: 36128015; PMCID: PMC9482787.
- Miravitlles M, Murio C, Guerrero T, Gisbert R; DAFNE Study Group. Decisiones sobre Antibioticoterapia y Farmacoeconomía en la EPOC. Pharmacoeconomic evaluation of acute exacerbations of chronic bronchitis and COPD. Chest. 2002 May;121(5):1449-55. doi: 10.1378/ chest.121.5.1449. PMID: 12006427.
- Miravitlles M, Solé A, Aguilar H, Ampudia A, Costa-Samarra J, Mallén-Alberdi M, Nieves D. Economic Impact of Low Adherence to COPD Management Guidelines in Spain. Int J Chron Obstruct Pulmon Dis. 2021 Nov 16;16:3131-3143. doi: 10.2147/COPD.S322793. PMID: 34848952; PMCID: PMC8611727.
- Müllerová H, Shukla A, Hawkins A, Quint J. Risk factors for acute exacerbations of COPD in a primary care population: a retrospective observational cohort study. BMJ Open. 2014 Dec 18;4(12):e006171. doi: 10.1136/ bmjopen-2014-006171. PMID: 25524545; PMCID: PMC4275672.
- Dharwal V, Paudel KR, Hansbro PM. Impact of bush-fire smoke on respiratory health. Med J Aust. 2020 Sep;213(6):284-284.e1. doi: 10.5694/mja2.50754. Epub 2020 Aug 30. PMID: 32862429.
- Beyene T, Harvey ES, Van Buskirk J, et al. ‘Breathing Fire’: Impact of Prolonged Bushfire Smoke Exposure in People with Severe Asthma. Int J Environ Res Public Health. 2022;19(12):7419. Published 2022 Jun 16. doi:10.3390/ ijerph19127419
- Davidsson T, Davidson JA, Banerjee A, Douglas I, et al. Primary prevention of acute cardiovascular events by influenza vaccination: an observational study. Eur Heart J. 2023;44(7):610-620. doi:10.1093/eurheartj/ehac737
Telehealth: remote monitoring of respiratory patients
The ability to monitor certain aspects of patients’ health from their home has become an increasingly popular telehealth option that have been accelerated by the COVID-19 pandemic1. Generally, telehealth spans from simple video calls between patients and doctors replacing routine visits to complex remote monitoring of general health or specific disease related parameters. Interestingly, telehealth as such have been shown to cut down on patients’ travel costs2 and infection risk at hospitals or in the GPs office3. But the overall health benefits are debated and a recent review of 29 studies utilizing remote monitoring in COPD care concluded that no important benefits for patients were obtained, neither looking at symptoms nor quality of life4. However, people who were monitored through telehealth technology and usual care had some reduction in risk of hospital re-admission4.
In COPD and asthma care, remote monitoring can largely be categorized based on the purpose of the monitoring:
- To predict or foresee flare ups by collecting health and disease parameters. This kind of monitoring is usually associated with simple monitoring such as QoL questionaries and health parameters as body temperature which is report digitally and monitored by nurses or potentially AI.
- To improve patient awareness of changes in symptoms by recording in digital diaries or mobile applications and thus realize potential triggers, which may lead to improved self-management.
- To improve care by increasing treatment adherence and or compliance, which usually involves the use of smart inhalers or add-on modules in connection with a mobile application displaying the data for the patient.
Despite the development of various digital tools such as mobile applications, smart inhalers, and smart add-on modules, a general implementation of these remains a challenge due to complexities in the use and the relative high cost that patients are reluctant to pay5. The cost related to remote monitoring and associated increased workload of analysing reports need to be studied to show that the use of these is cost effective, providing better disease control and improved quality of life for patients5.
Thus, having the purpose in mind when trying to identify patients where remote monitoring can add value seems to be key –when it comes to remote monitoring of patients there is no one size fits all!

Nicolai Krogh
Medical Science Liaison
References:
- Shilpa N. Gajarawala and Jessica N. Pelkowski. Telehealth Benefits and Barriers. The Journal for Nurse Practitioners 17 (2021) 218-221.
- Centaine L Snoswell, Monica L Taylor, Tracy A Comans, Anthony C Smith, Leonard C Gray, and Liam J Caffery. Determining if Telehealth Can Reduce Health System Costs: Scoping Review. J Med Internet Res. 2020 Oct; 22(10): e17298.
- Mai Tsutsui, Firoozeh Gerayeli, and Don D Sin. Pulmonary Rehabilitation in a Post-COVID-19 World: Telerehabilitation as a New Standard in Patients with COPD. Int J Chron Obstruct Pulmon Dis. 2021 Feb 19;16:379-391.
- Janjua S, Carter D, Threapleton CJD, Prigmore S, Disler RT. Telehealth interventions: remote monitoring and consultations for people with chronic obstructive pulmonary disease (COPD). Cochrane Database of Systematic Reviews 2021, Issue 7. Art. No.: CD013196.
- Henry Chrystyn, Raphaele Audibert, Manfred Keller, et al. Real-life inhaler adherence and technique: Time to get smarter! Respir Med. 2019 Oct-Nov;158:24-32.
GOLD guideline evolution: BC is out and Exacerbation prone is in
Reference to presentation: Current challenges in airways disease management – Evolution in GOLD: we cannot ‘see’ ‘C’ anymore and LABA/ICS are gone. Helpful or a hindrance?
Speaker: Antonio Anzueto, USA
When the first GOLD guideline document was released in 2001, the assumption was that poorer lung function led to poorer outcome. The best strategy was therefore thought to be a step-up approach where more pharmacotherapy was added depending on the severity of the lung function reduction.
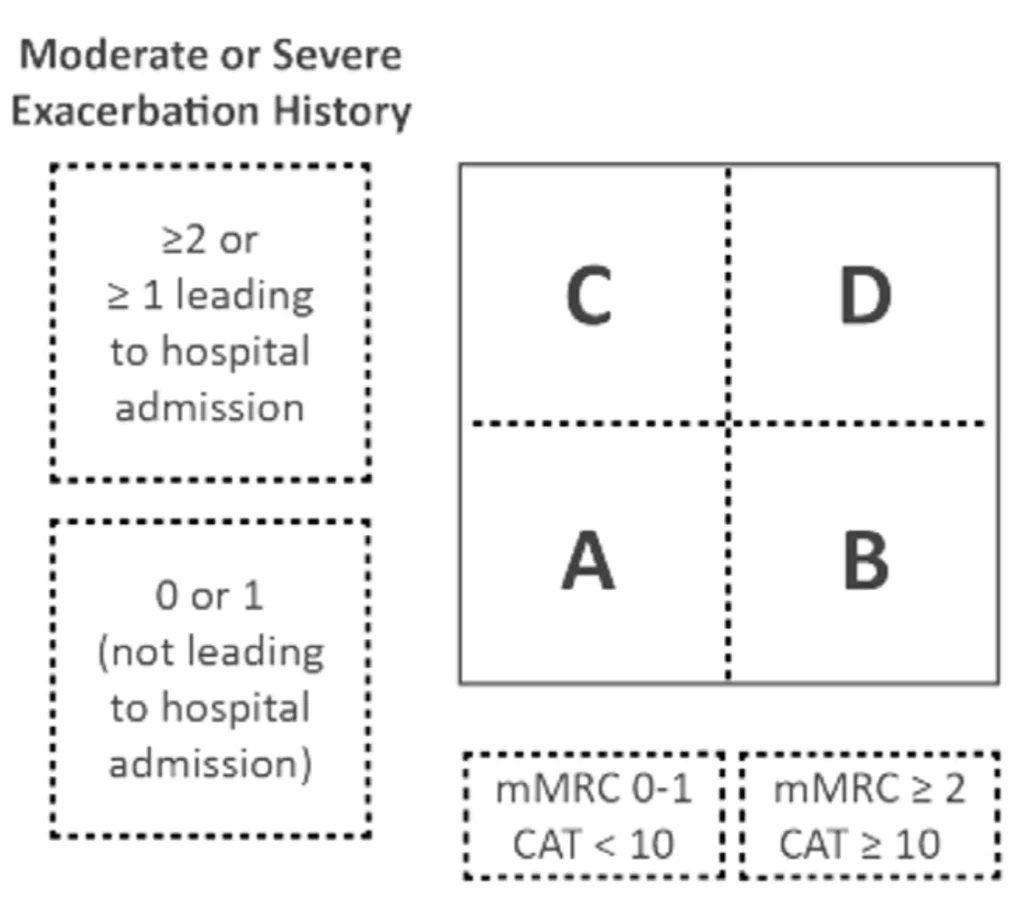
By 2015, data had accumulated showing that there was no association between the severity by lung function and symptoms evolution, risk of exacerbations or even outcomes. Data also clearly showed that there were means to prevent exacerbations and reduce symptoms. The GOLD committee decided to divide patients into four groups, ABCD (2015 Global Initiative for Chronic Obstructive Lung Disease).
Exacerbations – not just about lungs
It was not fully understood until recent years that exacerbations changes disease progression. It is now recognized that exacerbations are bad and should be prevented. They trigger more inflammations, accelerate decline in lung function, increase worsening of comorbidities1. Patients who are hospitalised due to exacerbation are significantly
at risk for cardiac events within the next 30 days. Exacerbations should be viewed in the light of the intimate interaction between lungs and the cardiovascular system.
There is strong data evidence to justify replacing the CD category with just E for Exacerbation prone patients, irrespective of symptoms. Whatever interventions done, they must address exacerbation risk.
State of the art COPD treatment – according to GOLD 2023
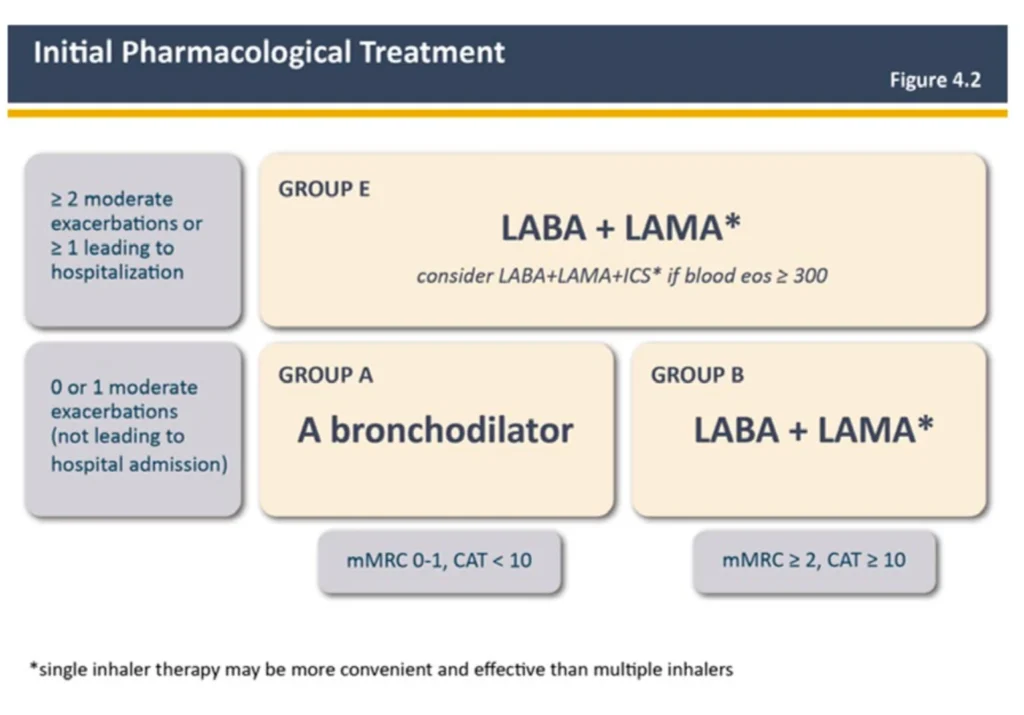
Based on the large amount of data gained in recent years to understand the role of bronchodilators, the committee decided to make following changes in GOLD 2023 guideline:
– “Initial therapy should consist of a LAMA+LABA combination…”
– “Consider LAMA+LABA+ICS combination if eos >300 cells/μL (practical recommendation…”
– “We do not encourage the use of LABA+ICS combination in COPD…”
– “If patients have COPD and concomitant asthma, they should be treated like patients with asthma…”
Gold 2023:
There are several publications showing that fixed LAMA/LABAs are better than ICS/LABA in lung function and reducing exacerbations.2,3,4
Use of ICS
Safety issues: Patients on ICS based medications that are still not getting any clinical benefit, may have increased risk for pneumonia due to the change of the airway microbiome5. Eosinophils may serve as biomarkers to indicate risk of pneumonia: a very low eosinophil count (<100 cells/μL) marks an increased risk.6
Place in therapy: ICS, together with bronchodilators, are intended to give maximum bronchodilation and anti-inflammation. Programs including thousands of patients in registration studies have demonstrated that these medications decrease exacerbations7. Exacerbations are known to be key drivers for mortality in COPD8.
Take-home message
1. We live in the golden era of COPD. More treatments are available now, compared to 20 years ago. New molecules are being developed and there is also a potential for biologics. The prospects are huge.
2. Exacerbations are bad – independent of the patient’s symptoms.
– Dual bronchodilators are the pivotal therapy9
– ICS should be used only in the context of triple therapy9
– Therapies are shaped by biomarkers and treatable traits

Pekka Ojasala
Medical Advisor
References:
- Flattet Y, Garin N, Serratrice J, Perrier A, Stirnemann J, Carballo S. Determining prognosis in acute exacerbation of COPD. Int J Chron Obstruct Pulmon Dis. 2017;12:467- 475. Published 2017 Jan 31. doi:10.2147/COPD.S122382
- Wedzicha JA, Banerji D, Chapman KR, et al. Indacaterol-Gly- copyrronium versus Salmeterol-Fluticasone for COPD. N Engl J Med. 2016;374(23):2222-2234. doi:10.1056/NEJMoa1516385
- Cazzola M, Page C, Rogliani P, Calzetta L, Matera MG. Dual bronchodilation for the treatment of COPD: From bench to bedside. Br J Clin Pharmacol. 2022;88(8):3657-3673. doi:10.1111/bcp.15390
- Vogelmeier C, Paggiaro PL, Dorca J, et al. Efficacy and safety of aclidinium/formoterol versus salmeterol/fluticasone: a phase 3 COPD study. Eur Respir J. 2016;48(4):1030- 1039. doi:10.1183/13993003.00216-2016
- Contoli M, Pauletti A, Rossi MR, et al. Long-term effects of inhaled corticosteroids on sputum bacterial and viral loads in COPD. Eur Respir J. 2017;50(4):1700451. Published 2017 Oct 5. doi:10.1183/13993003.00451-2017
- Martinez-Garcia MA, Faner R, Oscullo G, et al. Inhaled Steroids, Circulating Eosinophils, Chronic Airway Infection, and Pneumonia Risk in Chronic Obstructive Pulmonary Disease. A Network Analysis. Am J Respir Crit Care Med. 2020;201(9):1078-1085. doi:10.1164/rccm.201908-1550OC
- See corresponding SmPC for exacerbation risk reduction per product
- Soler-Cataluña JJ, Martínez-García MA, Román Sánchez P, Salcedo E, Navarro M, Ochando R. Severe acute exacerbations and mortality in patients with chronic obstruc- tive pulmonary disease. Thorax. 2005;60(11):925-931. doi:10.1136/thx.2005.040527
- Global Initiative for Chronic Obstructive Lung Disease 2023 [cited Sept 2023]. Available from: http://www.goldcopd.com/
Longitudinal cohorts in airway disease:
What have they taught us about personalised treatment of our everyday patients?
The importance and relevance of learnings from longitudinal studies was a topic in our previous issue of ERS congress report, and you can read more about the COPDGene and U-BIOPRED cohorts there. But because of its importance we wish to stay just a little longer on the subject.
The ATLANTIS1 study, aiming to assess the involvement of small airways in asthma, presented by Monika Kraft (NY, USA), collected data from mild to moderate asthmatics for 8 years. Already in 1996, Dr. Kraft demonstrated that inflammation exists throughout the whole branch of the lungs. The study shows that the distal lung can no longer be referred to as the silent zone. ATLANTIS was the first study to collect data in a bigger sample size (n=773 individuals). Over 90% of study subjects were shown to have at least one sign of small airway dysfunction amongst all different measures performed2. Physiological, but not CT measurements, are drivers for exacerbations, and oscillometry measurements are of value3. The ATLANTIS investigators hope to develop a single question-tool to be provided to clinicians that would allow identification of small airways dysfunction and with this, identifying who is at risk of exacerbations. Moreover, data from persons living with COPD is required.

A study cohort collecting real world evidence from asthma, COPD or combination of both, Alberto Papi (Cona, Ferrara, Italy) presented the 3 year long NOVELTY study4. The study starts from real life and physician’s diagnosis of disease, to thereafter break down the learnings into disease mechanisms5 and treatable traits.6 They are now starting to dig deeper into the molecular and underlying pathways and are hoping to present more insights characterizing new clinical endotypes within asthma and/or COPD. It will be exciting to see the future results of the study.

Barbara Fuchs
Medical Manager, Chiesi Nordics
References:
- Postma DS, Brightling C, Fabbri L, van der Molen T, Nicolini G, Papi A, Rabe KF, Siddiqui S, Singh D, van den Berge M, Kraft M. Unmet needs for the assessment of small airways dysfunction in asthma: introduction to the ATLANTIS study. Eur Respir J. 2015 Jun;45(6):1534-8. doi: 10.1183/09031936.00214314. PMID: 26028618.
- Postma DS, Brightling C, Baldi S, Van den Berge M, Fabbri LM, Gagnatelli A, Papi A, Van der Molen T, Rabe KF, Siddiqui S, Singh D, Nicolini G, Kraft M; ATLANTIS study group. Exploring the relevance and extent of small airways dysfunction in asthma (ATLANTIS): baseline data from a prospective cohort study. Lancet Respir Med. 2019 May;7(5):402-416. doi: 10.1016/S2213-2600(19)30049-9. Epub 2019 Mar 12. Erratum in: Lancet Respir Med. 2019 Sep;7(9):e28. PMID: 30876830.
- Kraft M, Richardson M, Hallmark B, Billheimer D, Van den Berge M, Fabbri LM, Van der Molen T, Nicolini G, Papi A, Rabe KF, Singh D, Brightling C, Siddiqui S; ATLANTIS study group. The role of small airway dysfunction in asthma control and exacerbations: a longitudinal, observational analysis using data from the ATLANTIS study. Lancet Respir Med. 2022 Jul;10(7):661-668. doi: 10.1016/S2213- 2600(21)00536-1. Epub 2022 Mar 2. PMID: 35247313.
- Golam SM, Janson C, Beasley R, FitzGerald JM, Harrison T, Chipps B, Hughes R, Müllerová H, Olaguibel JM, Raps- omaniki E, Reddel HK, Sadatsafavi M; NOVELTY study investigators. The burden of mild asthma: Clinical burden and healthcare resource utilisation in the NOVELTY study. Respir Med. 2022 Aug-Sep;200:106863. doi: 10.1016/j. rmed.2022.106863. Epub 2022 May 9. PMID: 35952579.
- Hughes R, Rapsomaniki E, Bansal AT, Vestbo J, Price D, Agustí A, Beasley R, Fageras M, Alacqua M, Papi A, Müllerová H, Reddel HK; NOVELTY Scientific Community; NOVELTY study investigators. Cluster Analyses From the Real-World NOVELTY Study: Six Clusters Across the Ast- hma-COPD Spectrum. J Allergy Clin Immunol Pract. 2023 Sep;11(9):2803-2811. doi: 10.1016/j.jaip.2023.05.013. Epub 2023 May 23. PMID: 37230383.
- Agustí A, Rapsomaniki E, Beasley R, Hughes R, Müllerová H, Papi A, Pavord ID, van den Berge M, Faner R; NOVELTY Study Investigators. Treatable traits in the NOVELTY study. Respirology. 2022 Nov;27(11):929-940. doi: 10.1111/ resp.14325. Epub 2022 Jul 21. Erratum in: Respirology. 2022 Dec;27(12):1095. PMID: 35861464; PMCID: PMC9795904.
Next generation evidence-based decision-making in respiratory medicine
A session exploring how real-life research may aid decision-making and guideline development and complement RCT for better assessment of interventions.
Bias, both in randomised controlled trials (RCT) and Real-world evidence (RWE) is important to minimize, as pointed out by Dr Giorgio Walter Canonica (Milan, Italy). RCTs, on one hand might target a very narrow treatment group to mitigate confounding factors, whereas in RWEs, subpopulation results might get lost in the heterogeneity of the real world. While evidence of efficacy is the strongest with RCT, the evidence of effectiveness, i.e. how well a treatment works in practice in a broader population, is better shown with RWE1. And thus, they complement each other, and both are needed.
Better use of real-world data
Aiming to raise the profile of real-life research, the Respiratory Effectiveness Group (REG) was formed. Together with EACCI (the European Academy of Allergy and Clinical Immunology), certain quality standards have been implemented. One point of action is to establish more registries for more systematic capture of real-world data2.
The REG and EAACI also organized a workshop in March this year to discuss integration of RWE and EBM (Evidence Based Medicine) into next generation guidelines, in which regulatory bodies such as the FDA and EMA participated, as well as patient organizations. A second workshop in October will finalize the outcomes of the first workshop.
mHealth – getting more health data from mobile devices
The WHO (world health organization) defines mHealth as medical and public health practice supported by mobile devices, (e.g. mobile phones or personal digital assistants)3. With the huge collection of data, big data processing and artificial

intelligence (AI) algorithms can be used for future evidence generation4, says Dr Hilary Pinnock (Edinburgh, UK). Still, only a minority of mHealth is embedded in routine healthcare5, although an increase has been seen from 2010 and accelerated by the COVID pandemic. While traditional healthcare data collects data at visits, mHealth has the potential to capture so much more data over the course of an illness and/or a lifetime. EAACI lists a number of areas, e.g. epidemiology, health economics, public health, where mHealth can be of help.
Do mHealth data represent everyone in the real world?
There is a risk that patient tools might attract a specific “type” of patient. In a study to demonstrate pollen and wildfire impact on asthma symptoms, predominantly white, male colleague students with high income signed up – however women over 40 were more likely to keep reporting data. Out of 7593 enrolled, only 64 and 37 respectively, logged persistent data throughout the study period.6 So what happens, if we use biased limited data to train AI?
Use of automated feedback, like wearable devices may provide data that is more generalizable. Integration of these systems into routine practice is also a task for policy makers and administrators. We have a long way to go, concludes Dr Pinnock, before we are generating data evidence well from mobile devices and mHealth tools.

Christina Eliasson
Nordic Product manager
References:
- Paoletti G, Pepys J, Casini M, et al. Biologics in severe asthma: the role of real-world evidence from registries. Eur Respir Rev. 2022;31(164):210278. Published 2022 Jun 7. doi:10.1183/16000617.0278-2021
- Di Bona, D., Paoletti, G., Chu, D.K., Pepys, J., Macchia, L., Heffler, E. and Canonica, G.W. (2021), Allergen immunotherapy for respiratory allergy: Quality appraisal of observational comparative effectiveness studies using the REal Life Evidence AssessmeNt Tool. An EAACI methodology committee analysis. Clin Transl Allergy, 11: e12033. https://doi.org/10.1002/clt2.12033
- WHO Global Observatory for eHealth. (2011). mHealth: new horizons for health through mobile technologies: second global survey on eHealth. World Health Organization. https://apps.who.int/iris/handle/10665/44607
- World Health Assembly, 71. (2018). mHealth: use of appropriate digital technologies for public health: report by the Director-General. World Health Organization. https://apps. who.int/iris/handle/10665/276430
- World Health Organization. (2016). Global diffusion of eHealth: making universal health coverage achievable: report of the third global survey on eHealth. World Health Organization. https://apps.who.int/iris/handle/10665/252529.
- Chan YY, Wang P, Rogers L, et al. The Asthma Mobile Health Study, a large-scale clinical observational study using ResearchKit. Nat Biotechnol. 2017;35(4):354-362. doi:10.1038/nbt.3826
HOT TOPICS:
Burden of tobacco farming and use of electronic nicotine delivery system on the environment and occupational health
Even the tobacco industry acknowledges the harm in smoking and claims to make efforts to transform by reducing health impacts of its products. The solution – as proposed by tobacco companies is not to end nicotine use but switching users to e-cigarettes. The e-cigarette market is growing rapidly but more typically from attracting new users than switching old smokers. Vaping is also where the industry sees its future growth, especially if combined with cannabis. Several of the biggest tobacco companies are investing in the cannabis industry – both medical and recreational use.
Vaping is not harmless. Combustible cigarettes and e-cigarettes, with or without nicotine, increases the resistance of small airways and decreases small airway function1. Sven-Erik Jordt, USA, presented findings from Duke University, that most of the available e-liquid products contain synthetic cooling agents. Addition of menthol is regulated in many markets since its cooling and pleasant sensory effects facilitate smoking and tobacco product initiation. However, since these derivates are without flavor, these may bypass regulatory limits on menthol content in tobacco products as they may not qualify as “characterizing flavor”. This is a potential regulatory loophole that should be considered, especially since health effects of inhaling these compounds are not fully known.
Environmental burden
Beyond the direct health impact cigarettes have on consumers, the lifecycle impacts on the environment are considerable: from deforestation for agriculture of the sensitive tobacco plant that requires heavy use of fertilizers and pesticides, and burning biomass for tobacco curing, to the post-consumer waste with cigarette butts ending up in the oceans, poisoning water.
Greenwashing the industry
To counteract the bad PR and divert attention from the harm done both from manufacturing and consumption of cigarettes, several tobacco companies are establishing an ESG concept (environmental, social and governance for sustainable development) to appear “green” and ethical. They are playing the game to keep investors and succeeding at it. For instance, Philip Morris Industry managed to get a high score on the Dow Jones Sustainability index. The tobacco companies also portray themselves as socially conscious, making charitable contributions, especially in LMIC (low-middle income countries). Labelling tobacco companies as philanthropists: That’s rich coming from an industry that sells a product that kills half of its long-time users, says Elif Dagly (Turkey).
The prevalence of smoking tobacco has unfortunately not been a positive development: The number of smokers globally increased from 0.99 billion in 1990 to 1.14 billion in 2019, most of them coming from LMIC countries. Globally in 2019, smoking tobacco use accounted for 7.69 million deaths and 200 million disability adjusted life years.2
In the final comment on the global burden of tobacco use, Om Prakash Kurmi of the Coventry University, UK concluded that the smoking epidemic is far from over.
The good news, however, is that health benefits come quickly on smoking cessation and life expectancy is increased – it is never too late to stop smoking.

Erika Petersson
Medical Digital Content Manager, Chiesi
References
- Hauck AS, Buchwald I, Watz H, Trinkmann F, Söling C, Ra- benstein A, Ruether T, Mortensen K, Drömann D, Franzen KF. Impact of Chewing Bags, E-Cigarettes, and Combust- ible Cigarettes on Arterial Stiffness and Small Airway Function in Healthy Students. Toxics. 2023 Jan 14;11(1):77. doi: 10.3390/toxics11010077. PMID: 36668804; PMCID: PMC9866725.
- GBD 2019 Tobacco Collaborators. Spatial, temporal, and de- mographic patterns in prevalence of smoking tobacco use and attributable disease burden in 204 countries and territories, 1990-2019: a systematic analysis from the Global Burden of Disease Study 2019 [published correction appears in Lancet. 2021 Jun 19;397(10292):2336]. Lancet. 2021;397(10292):2337-2360. doi:10.1016/S0140-6736(21)01169-7.
Warm greetings from Milan!
There is a difference between weather and climate, but still, one cannot help wondering if the current temperatures in Milan around 30 degrees is not to underline what a hot topic global warming is. The congress theme is Pollution, climate change and sustainable developments and the aim has been to integrate these themes as broadly as possible. The interconnection between planet health and respiratory health is becoming more and more evident. Pollutants are not only a health hazard, but many pollutants are also sources of high CO2 emissions1. Use of fossil fuels causes both particulate matter and CO2. We breathe climate change, and addressing emissions will benefit both planet and human health.

So, the elephant-in-the-room-question came up in a symposium about pollution and climate changes: how do we justify flying thousands of participants from around the world for a congress? The response from the panel was that ERS will continue to offer hybrid congresses for environmental reasons, to recommend travelling by train where feasible and by proposing climate compensation for those who fly. This will leave Milan with more trees after the congress. Frequency of global conferences can of course also be reassessed, but it is difficult to get the same interaction and sense of engagement from online participation, and close to impossible to get the same opportunities of collegial interaction and unexpected conversations in any other way than to meet as a community.
As a community, the health care sector can utilize its credibility to put pressure on policy makers to take action to reduce air pollution. Maria Neira, WHO, urged the audience to be very cautious about terminology and to be strategic about using positive arguments for the health benefits of fighting air pollution. Strategy is vital because, as she pointed out, before we had ONE industry to fight (referring to the tobacco industry) whereas now, the health threats related to emissions are coming from all sectors – including health care.
To improve air quality is to reduce future healthcare costs related to treating preventable diseases.

Erika Petersson
Medical Digital Content Manager, Chiesi Nordic
Reference
- Air pollution (who.int) internet page visited September 11, 2023
Pulmonary rehabilitation in severe and very severe COPD.
At the Sunday session “Targeting treatable traits in severe chronic obstructive pulmonary disease: a nonpharmacological approach”, we got an update on ‘treatable traits’ for advanced COPD patients beyond ‘regular care’. There was a consensus throughout the session that we should regard the COPD patients as more than the diseased lung. Evidence evolved during the past decade shows that severe COPD patients benefit a lot from pulmonary rehabilitation programs. Frits M.E. Franssen from the Netherlands provided us with up-to-date insights on how to rehabilitate a severe COPD patient.
Franssen presented the definition of pulmonary rehabilitation as a comprehensive intervention based on a thorough patient assessment followed by patient tailored therapies. The aim of pulmonary rehabilitation is to improve the physical and psychological condition of patients, not only with COPD but also with other chronic respiratory diseases, as well as to promote a healthy lifestyle. There is an ongoing international debate about the core components of pulmonary rehabilitation. It is important to remember, says Franssen, that pulmonary rehabilitation is more than exercise training and education. If we look at the needs of individual patients, interventions like nutritional support, psychological support, lifestyle interventions, optimization of pharmacotherapies and adherence to medication and advanced care planning are also components with potentially large benefits. Looking closer at the benefits, most evidence is on improvement of exercise tolerance, reduction in shortness of breath and improvement in quality of life1.
However, studies also show that other important outcomes of pulmonary rehabilitation include improvement in body composition, reduction in psychological symptoms and reduction in mortality and re-admissions. Looking further into patient groups, hyperinflation is associated with dyspnoea, therefore patients with severe hyperinflation could be prevented from exercising to a sufficient level. Interestingly, when targeting specifically at this group of patients, Vanfleteren and colleagues (Vanfleteren et al., Arch Phys Med Rehabil 2018) demonstrated that static lung hyperinflation does not prevent patients from benefiting from pulmonary rehabilitation.

Ingvild Bjellmo Johnsen
Medical Advisor Respiratory, Chiesi Nordic
Reference:
- McCarthy et al., Cochrane Syst Rev. 2015, Maltais et al., Am J Respir Crit Care Med 1996, Lindenauer et al., JAMA 2020, Schois et al., A J Respir Crit Care Med 1998, Maddocks et al., Thorax 2016, Coventry et al. J Psycsom Res 2007, Stoilkova et al., Respir Med 2013, vivodlzev et al., CHEST 2010, Moore et al., CHEST 2017, Stefan et al., Am J Respir Crit Care Med 2021, Pitta et al, CHEST, 200
Improving respiratory care from a primary care perspective
Sustained health system benefits of primary care based integrated disease management for COPD: an interrupted time series
Severe exacerbations in patients with chronic obstructive pulmonary disease (COPD) is a challenge for both patient and health care system. Methods to prevent exacerbations are therefore needed.
To evaluate whether a primary care integrated disease program (IDM) can reduce health service utilisation, patients with severe COPD were studied in a real-world setting. All individuals managed by the Best Care program (2011-2019, Ontario Canada) with a clinical diagnosis of COPD were included (N=2451, mean age 67 years, female rate 48.3). Primary endpoint was COPD-related hospital admissions and COPD related ED visits, and the secondary endpoint was all cause hospitalizations and admissions and all-cause ED visits.
Best Care COPD is built around a triad of health care stakeholders including the patient/caregiver, the primary care provider, and a certified respiratory educator. The program is located at the primary care provider clinic and consists of a set of structured intervention including:
- assessment
- education
- self-management
- medication management
- skills training
- evaluation
Through an interrupted time series analysis of retrospective administrative data, the study assessed the number of COPD-related and all-cause hospital admissions and emergency department (ED) visits 36 month pre- and post IDM program initiation. IDM program patients were linked to administrative health databases in the study amassing 13,000 person years of follow-up. In the year prior to commencing IDM, 9.2% of individuals experienced a total of 383 COPD related hospitalisations, and 20.4% individuals generated 809 COPD-related ED visits.

The study found that the monthly rate of COPD related hospitalisation and ED-visits in 1000 individuals 12 month after program initiation was decrease by 9.1 and 19.0 respectively, corresponding to a relative reduction of 56% and 46%. After 36 months, monthly rate of events per 1000 individuals almost halved.
The study concluded, said presenter Christopher Licskai, that primary care-based COPD IDM program was associated with significantly improved disease trajectory, and reduced COPD related and all-cause ED visits and hospitalisation.

Sarah Friberg,
Value and access director
Recommended reading
- Global initiative for chronic obstructive lung disease. Global strategy for the diagnosis, management and prevention of chronic obstructive lung disease. Report;2023
- Criner GJ, et al. Prevention of acute exacerbations of thoracic obstructive pulmonary disease: American College of Chest Physicians and Canadian Thoriacic Society Guideline. Chest. 2015;147(4):894-942
- Poot CC, Meijer E, Kruis AL, Smidt N, Chavannes NH, Honkoop PJ. Integrated disease management interventions for patients with chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2021;9(9):CD009437. Published 2021 Sep 8. doi:10.1002/14651858.CD009437.pub3
References:
Ferrone M, et al. The impact of integrated disease management in high-risk COPD patients in primary care. Npj Prim Care Respir Med. 2019;29(1):8
Improving respiratory care from a primary care perspective.
A systematic review of methods of scoring inhaler technique.
For many decades, inhalers have been used to treat respiratory diseases. However, a recent study has shown that correct inhaler technique (IT) is becoming poorer and contributes to reduction in disease control¹.
A team of researchers from the UK came to realize that, to date, there were no known scoring systems to assess and quantify inhaler technique. In medicine, scoring systems are widely used and scoring IT has been observed as an outcome measure within research studies. Hence, the investigators conducted a systematic review to collate and evaluate methods of scoring IT in research literature.
Methodology:
- The literature search was conducted through EMBASE, MEDLINE, CINAHL, PubMed, BNI google scholar and citation searching.
- Asthma and COPD was the terms that the search was centred around.
- Use of score as an outcome to measure of inhaler technique was the eligible criteria for the publications included in the search.
- 77 articled was included in the systematic review
Articles were categorised and grouped according to the method of scoring IT and 6 themes identified;
- awarding 1-point per step
- grading final score
- points deducted from final scoring method
- expressing total score as a percentage
- weighting steps within the checklist
- “validated” scoring methods
All of the above mentioned methods brought challenges and uncertainties such as no consensus on score interpretation, complex and time consuming etc. For the investigators, this confirmed an unmet need for a validated scoring system to assess IT in clinical practice.
Investigator’s wish list for a scoring tool:
- A standardised and content valid IT checklist
- Robust validation processes to ensure the tool measures IT and highlights poor technique
- A score yielding a meaningful outcome that can facilitate IT optimisation
A validated measurement tool, applicable to all inhaler device types, would, if available, be useful in clinical practice to better assess, measure, and optimise patient’s inhaler technique.

Maria Messerer, PhD
Medical Director, Chiesi Nordic
References:
1J. Sanchis. Chest 2016. 150 (2).394-406
Longitudinal cohorts in airway disease:
What have they taught us about personalised treatment of our everyday patients?
Longitudinal cohorts in airway disease: What have they taught us about personalised treatment of our everyday patients?
Due to the nature of longitudinal studies, the data and learnings obtained are as plenty as they are important and relevant. This became very clear when attending the session covering four longitudinal studies from the field of asthma and COPD. During the discussions, it was also underlined that no trivial baseline characterisation of cohorts in clinical trials can be allowed in future to be able to see the full picture.
Kian Fan Chung (London, UK) shared insights from the U-BIOPRED cohort, investigating Unbiased Biomarkers for the Prediction of Respiratory Disease Outcomes.
Read more about the study and its results on the homepage of the Innovative Medicine Initiative, https://www.imi.europa.eu/projects-results/project-factsheets/u-biopred).

Here, system biology was applied to reveal mechanisms of severe asthma. This resulted in the definition of several clusters, each comprising a distinct phenotype of the disease. One of the discovered clusters of biomarkers include the combination of blood eosinophils and fraction of exhaled nitric oxide, FeNO to be able to detect the IL-13 Type2 hi phenotype1. Other clusters of biomarker combination define phenotypes of disease including “T2 low/non-T2”, which can either involve inflammasomes, Interferons and tumor-necrosis factor, or show signs of oxidative stress and aging, while being paucigranulocytic.
Moreover, the role of mast cells in asthma was confirmed, and the importance of distinguished activation2 pathways, i.e. via IgE-receptor activation or Interleukin-33-receptor activation. Results from the U-BIOPRED cohort also identified interleukin-6 as a potentially important pharmaceutical target for a cluster of “IL-6 Transsignalling high” severe asthmatics3.
The COPDGene study was presented by MeiLan Han (Ann Arbor, USA). Initially set-up to investigate underlying genetic factors of COPD, this study currently collects data from the 15 year follow-up. Although this cohort of n=5564 subjects identified a list of genetic loci associated with COPD4 (Hobbs Nat Gen 2017), it is still a mystery how these genes influence COPD genesis, Dr. Han says. The impact of genes appears rather small and is only detectable if genes are combined. The cohort also found a group of subjects not fulfilling the diagnostic criteria of COPD, which nevertheless have symptoms, exacerbations and radiographic abnormalities5. Dr. Han refers to the “myth of the healthy smoker”.
The COPDGene cohort also collected data on the causes of deaths occurring and found that these differ between different GOLD stages. Milder disease leads to death by cardiovascular causes and lung cancer, while patients in GOLD 3 and 4 decease in respiratory failure.
Finding from the cohort actually led to changes in routines at in Michigan, USA: from CT scans, a PA:A enlargement is an indicator for increased risk of exacerbations and is now included in the CT report. Moreover, small airways disease is identified as a precursor for emphysema and now reported if present on CT scans.

Barbara Fuchs,
Medical Manager, Chiesi Nordic
References:
1Pavlidis S, Takahashi K, Ng Kee Kwong F, et al. «T2-high» in severe asthma related to blood eosinophil, exhaled nitric oxide and serum periostin. Eur Respir J. 2019;53(1):1800938. Published 2019 Jan 3. doi:10.1183/13993003.00938-2018
2Tiotiu A, Badi Y, Kermani NZ, et al. Association of Differential Mast Cell Activation with Granulocytic Inflammation in Severe Asthma. Am J Respir Crit Care Med. 2022;205(4):397-411. doi:10.1164/rccm.202102-0355OC
3 Jevnikar Z, Östling J, Ax E, et al. Epithelial IL-6 trans-signaling defines a new asthma phenotype with increased airway inflammation. J Allergy Clin Immunol. 2019;143(2):577-590. doi:10.1016/j.jaci.2018.05.026
4Hobbs BD, de Jong K, Lamontagne M, et al. Genetic loci associated with chronic obstructive pulmonary disease overlap with loci for lung function and pulmonary fibrosis. Nat Genet. 2017;49(3):426-432. doi:10.1038/ng.3752
5Regan EA, Lynch DA, Curran-Everett D, et al. Clinical and Radiologic Disease in Smokers With Normal Spirometry [published correction appears in JAMA Intern Med. 2015 Sep;175(9):1588]. JAMA Intern Med. 2015;175(9):1539-1549. doi:10.1001/jamainternmed.2015.2735
Word of the day:
Have you heard about Syndemic Diseases yet?
- Most persons living a life with COPD have at least one additional, clinically relevant chronic disease
- Many chronic diseases have shared risk factors, e.g. aging, smoking, pollution, physical inactivity, and poverty
- Co-occurring diseases potentially share pathobiological mechanisms
- The term “syndemic” is used to describe the co-occurrence of diseases with shared mechanisms and risk factors
- Approaching syndemic diseases including COPD in the multimorbid stage clinically could lead to more patient-centric rather than a single-disease approach to therapy
Learn more about COPD and multimorbidity: recognising and addressing a syndemic occurrence here!
https://doi.org/10.1016/S2213-2600(23)00261-8 (published in Lancet Respiratory Medicine, Sept 8 2023)



