Supporting Patients to Manage their Asthma
Speaker: Liz Steed, Reader in Health Psychology, Queen Mary University of London, UK
In summary: Except for the few hours spent on the clinic, the patients relily on self-managing their disease practically all hours of the year, making it important to understand the drivers of the asthma patient’s behaviour, patient perspectives and treatment beliefs.
How much time do patients spend self-managing?
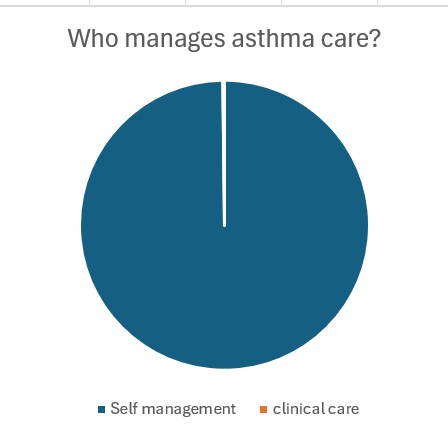
Given 8760 hours per year and 2-25 hours with clinician;
- 99.9% of time is self-management
Supported self-management is recommended in GINA
GINA report 2024 commands making an Asthma Action Plan: Assess, Adjust when needed and Review accordingly. Supported self-management is associated with significantly improved clinical and quality of life outcomes, hospitalizations, emergency visits and unscheduled consultations1. In self-management, 14 distinct variables have been identified and include supporting adherence, training, education and social support.2 It is important to understand the drivers of the asthma patient’s behaviour, patient perspectives and treatment beliefs.
What do we know about behaviour in asthma?
- 70% of the patients lack an action plan3
- Medication adherence varies between 22-78%
- 31% of patients rely on reliever inhalers3
- App. 20% of the asthma patients smoke4
- Fewer exercise – people with asthma are more sedentary and less physically active than those without. 5
- Uptake of vaccines is app. 40% 6
Several qualitative barriers impact self-management
Effective self-management may be hindered by misconceptions about asthma and poor understanding of asthma care. Social support, co-morbidities, access to healthcare and doctor-patient relationship also play a role.7
Facilitating self management
The understanding of illness beliefs is essential. The impact that health beliefs can have on behaviour around asthma itself and its treatment can, in fact, may be more important to address than functional measures of airway obstruction.
Good patient education is key and needed8 – and digital tools and intervention may be helpful. It is also important to acknowledge that adult patients that have been suffering from asthma since childhood may not have had any additional training as adults.
Common asthma myths leading to undertreatment
- ‘Asthma is acute’ – no symptoms, no asthma!
- ‘Good control includes some symptoms’
- ‘Mild asthma isn’t serious’
Clinicians recognize asthma as a chronic condition, but the patients are far more likely to perceive asthma as an acute illness – only present when symptoms occur, thus prioritizing acute reliever medication over preventive medication. All severities of asthma can be serious/fatal – it is serious and needs treatment. Patients need a better understanding of what good control looks like and when to seek care if they don’t have it.
Consider the phsycological impact of asthma
Anxiety prevalence is nearly two-fold in asthma patients compared to non-asthmatics. This is important to assessed and managed.9
How do we support the asthma patients best?
- Regular reviews (minimum 2 hours annually to establish self-management skills) reduce unscheduled healthcare use.10
- Consider timing of annual reviews for those with seasonal triggers.
- Complex disease may require multidisciplinary case management
- Unsupported or minimally supported self-management programs are not effective.
Partnering with the patient and implementing shared decision making requires understanding the drivers of behaviour but is important in improving self-management of asthma.
Take home messages:
- Patients are managing but support from healthcare can make a difference
- Asthma requires multiple behaviours and ‘work’ within a social/cultural environment.
- Behaviour is dynamic and complex
- Understanding behaviour change and self-management models can help.
’We can have all the scientific developments in the world, but if we don’t listen to and hear our patient’s beliefs and concerns, they are not going to have the impact we would like them to.’
Liz Steed
References:
- Pinnock H, Parke HL, Panagioti M, et al. Systematic meta-review of supported self-management for asthma: a healthcare perspective. BMC Med. 2017;15(1):64. Published 2017 Mar 17. doi:10.1186/s12916-017-0823-7
- Taylor SJC, Pinnock H, Epiphaniou E, et al. A rapid synthesis of the evidence on interventions supporting self-management for people with long-term conditions: PRISMS – Practical systematic Review of Self-Management Support for long-term conditions. Southampton (UK): NIHR Journals Library; December 2014.
- Asthma and Lung UK, press release, 24th April 2024. Page visited March 10, 2025. https://www.asthmaandlung.org.uk/media/press-releases/asthma-care-crisis-charity-sounds-siren-asthma-death-toll-rises
- Thomson NC, Polosa R, Sin DD. Cigarette Smoking and Asthma. J Allergy Clin Immunol Pract. 2022;10(11):2783-2797. doi:10.1016/j.jaip.2022.04.034
- Urroz Guerrero PD, Oliveira JM, Lewthwaite H, Gibson PG, McDonald VM. Key Considerations When Addressing Physical Inactivity and Sedentary Behaviour in People with Asthma. J Clin Med. 2023 Sep 15;12(18):5998. doi: 10.3390/jcm12185998. PMID: 37762938; PMCID: PMC10531510.
- Keenan H, Campbell J, Evans PH. Influenza vaccination in patients with asthma: why is the uptake so low? Br J Gen Pract. 2007 May;57(538):359-63. PMID: 17504585; PMCID: PMC2047009.
- Miles C, Arden-Close E, Thomas M, Bruton A, Yardley L, Hankins M, Kirby SE. Barriers and facilitators of effective self-management in asthma: systematic review and thematic synthesis of patient and healthcare professional views. NPJ Prim Care Respir Med. 2017 Oct 9;27(1):57. doi: 10.1038/s41533-017-0056-4. PMID: 28993623; PMCID: PMC5634481.
- Daines L, Morrow S, Wiener-Ogilvie S, Scott C, Steed L, Taylor SJ, Pinnock H. Understanding how patients establish strategies for living with asthma: a qualitative study in UK primary care as part of IMP2ART. Br J Gen Pract. 2020 Apr 30;70(694):e303-e311. doi: 10.3399/bjgp20X708869. PMID: 32205333; PMCID: PMC7101272.
- Ye G, Baldwin DS, Hou R. Anxiety in asthma: a systematic review and meta-analysis. Psychological Medicine. 2021;51(1):11-20. doi:10.1017/S0033291720005097
- McClatchey K, Hammersley V, Steed L, et al. IMPlementing IMProved Asthma self-management as RouTine (IMP2ART) in primary care: study protocol for a cluster randomised controlled implementation trial. Trials. 2023;24(1):252. Published 2023 Apr 3. doi:10.1186/s13063-023-07253-9
ID13875-13.03.2025